The Philippine Health Insurance Corporation (PhilHealth) assure all members and their qualified dependent women, who are about to give birth, may avail themselves of PhilHealth benefits, up to 4th delivery, as well as Babies of members are also assured of the Newborn Care Package (NCP).
For clarification, PhilHealth Maternity Benefits categorized into two packages:
- Maternity Care Package (MCP) – PhilHealth benefit for the coverage of the first four births in accredited non-hospital facilities like birthing homes, lying-in, midwife managed clinics.
- Normal Spontaneous Delivery (NSD) Package – is the benefit provided by PhilHealth for the coverage of normal deliveries of the first four births in accredited hospitals.
What is Maternity Care Package?
The Maternity Care Package (MCP) are health services during antenatal period, normal delivery and post-partum period, including follow-up visits within 72 hours and one (1) week after delivery.
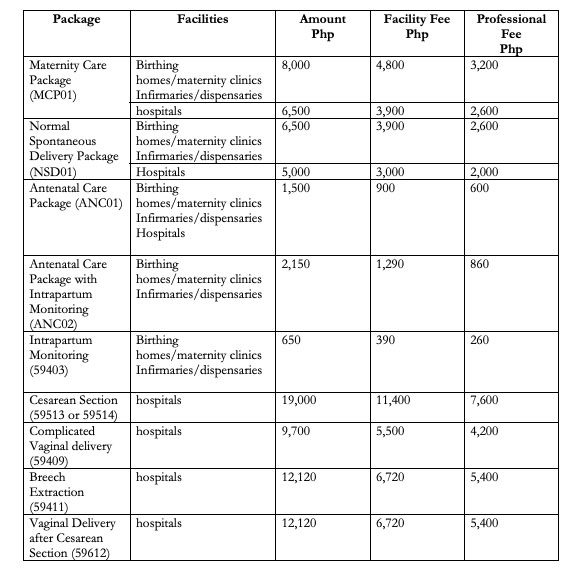
The MCP is worth PhP6,500 if availed of in an accredited hospital and PhP8,000 when availed of in accredited birthing homes, maternity clinics, infirmaries or dispensaries.
Benefit Availment Maternity Care Package Requirements
- Claim form 1
- Claim form 2
- Claim form 3 (part II)
- Updated Member Data Record (MDR)
- proof of eligibility
- (a) sponsored ID, (b) OWP ID, (c) IPP – proof of premium payments
- File within 60 days after the delivery
Included in the MCP are health services during antenatal period, normal delivery, and post-partum period, including follow-up visits within 72 hours and one (1) week after delivery. The MCP is worth PhP6,500 if availed of in an accredited hospital and PhP8,000 when availed of in accredited birthing homes, maternity clinics, infirmaries, or dispensaries.
Who can avail
- Members and qualified dependents (Up to 4th delivery only)
- Contribution requirements
Who provides
- Non-hospital facilities
- Engaged Maternity and Lying-in Clinics
- Engaged physicians and midwives
What services
- Prenatal care
- Delivery
- Post-natal care
Important Features:
- P 1,500 pre-natal care fee
- P 6,500 facility fee including professional fee
- No balance billing
- Applicable to Normal spontaneous vaginal deliveries performed in a non-hospital facility (birthing homes, lying-in, midwife managed clinics)
- Covers first 4 normal spontaneous deliveries
Inclusion
- Normal (uncomplicated) vaginal deliveries
- Low risk at the start and throughout labor and delivery
- Infant in vertex position
- Infant in 37 to 42 weeks AOG
- 1st pre-natal check-up must not exceed 16 weeks AOG
Exclusion
- 5th and subsequent deliveries
- Maternal conditions that are considered high risk as enumerated in Circular 20, s 2008
Maternity Care Package Excluded Maternal Conditions
- Age less than 19y/o
- First pregnancy at the age of 35 or greater
- Multiple pregnancy
- Ovarian abnormality (ovarian cyst)
- Uterine abnormality (myoma uteri)
- Placental abnormality (placenta previa)
- Abnormal fetal presentation (ie breech)
- History of 3 or more abortions/miscarriage
- History of 1 stillbirth
- History of major obstetric/gynecologic surgical operations (ie CS, uterine myomectomy)
- History of medical conditions (hypertension, pre-eclampsia, thyroid disorder)
- Other risk factors that warrant referral for further management (ie premature contractions, vaginal bleeding)
What is Normal Spontaneous Delivery Package (NSD)?
This package is applicable to all PhilHealth accredited hospital or non-hospital facilities like maternity and lying-in clinics. It includes prenatal care, delivery, and postnatal care services such as the following:
- ₱1,500.00 prenatal care free
- ₱5,000.00 to ₱6,500.00 facility fee including professional fee
- NO balance billing (applies to all)
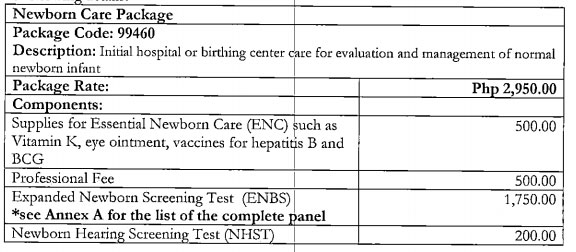
Newborn Care Package
As stated in (Circular Nos. 24 s. 2006 and 20 s. 2007) may be availed by any qualified PhilHealth dependent delivered in accredited hospitals and non-hospital facilities for MCP that is certified as a newborn screening facility.
This package is applicable to all PhilHealth accredited hospital or non-hospital facilities like maternity and lying-in clinics. The Newborn Care Package is worth ₱1,750.00 with NO billing balance. It includes prenatal care, delivery, and postnatal care services such as the following:
- Screening test – newborn screening and hearing
- Essential Intrapartum and Newborn Care (EINC) protocol
- non-separation of mother/baby for early breastfeeding initiation
- eye prophylaxis
- weighing
- BCG Vaccination
- Hepatitis B Vaccination
- Newborn Hearing Test
- Newborn Screening Test
- Professional fee
Please refer to the table below:
Source: PhilHealth